
Diabetes is a disorder in which the body does not produce enough insulin or does not utilize insulin properly. Insulin is a hormone that allows sugar to enter cells, where it can be turned into energy. In untreated diabetes, high levels of sugar can accumulate in the blood and damage organs, including blood vessels, eyes and kidneys. Some individuals with diabetes need daily insulin injections to prevent these complications.
About one in I00 women of childbearing age has diabetes before pregnancy (preexisting diabetes). Another 2 to 5 percent develop diabetes during pregnancy (gestational diabetes). In both forms, it is crucial to control blood sugar levels to reduce risks to the pregnant woman and her fetus.
Fetal Risks
Women with poorly controlled pre-existing diabetes in the early weeks of pregnancy are several times more likely than nondiabetic women to have a baby with a serious birth defect, such as a heart defect or neural tube defect (NTD – birth defect of the brain or spinal cord). They also are at increased risk of miscarriage and stillbirth.
Women with gestational diabetes, which generally develops later in pregnancy, usually do not have an increased risk of having a baby with birth defects. However, some studies suggest that, if a woman’s gestational diabetes is severe enough to require treatment with insulin, her baby may be at increased risk of birth defects. It is possible that some of the women may have had unrecognized diabetes that began prior to pregnancy. They may have had high blood sugar levels in the early weeks of pregnancy, which increases the risk of birth defects.
Poorly controlled gestational diabetes also slightly increases the risk of still-birth. However, with improvements in medical care, stillbirth is rare.
Women with poorly controlled diabetes are at increased risk of having a very large baby ( 10 pounds or more).
Macrosomia is the medical term for this. These babies grow so large because some of the extra sugar in the mother4 s blood crosses the placenta and goes to the fetus. The fetus then produces extra insulin, which helps it process the sugar and store it as fat. The fat tends to accumulate around the shoulders and trunk, sometimes making these babies difficult to deliver vaginally and putting them at risk for injuries during delivery.
Pregnancy Complications
With advances in medical care, women with diabetes are almost as likely as women without diabetes to have an uncomplicated pregnancy and a healthy baby, as long as blood sugar levels are wen controlled beginning prior to pregnancy. However, women with poorly controlled diabetes, especially preexisting diabetes, are at increased risk of certain. pregnancy complications. These include: miscarriage; pregnancy-related high blood pressure; polyhydramnios (an excess of amniotic fluid, which can contribute to preterm labor); preterm delivery; and stillbirth.
Preexisting Diabetes and Preconception Care
Women with preexisting diabetes should consult their doctors before pregnancy to ensure that their blood sugar levels are well controlled. This is important because the most serious birth defects associated with diabetes originate in the early weeks of pregnancy, before a woman may realize she is pregnant.
Women with preexisting diabetes who take oral medications to control their blood sugar levels will need to switch to insulin before conceiving and during pregnancy, as the oral medications may pose a risk of birth defects.
Screening for Gestational Diabetes
Gestational diabetes is one of the most common complications of pregnancy. It usually develops during the second half of pregnancy, when hormones interfere with the body’s ability to use its insulin.
Women at increased risk of gestational diabetes include: those who are over age 30; are obese; have a family history of diabetes; or have had a very large (over 9 l/2 pounds) baby or a stillborn.
The test involves taking a blood sample one hour and two hours after consuming a drink of 75 grams of glucose.
Once gestational diabetes is diagnosed, most women can control their blood sugar levels with diet, although about 10 to 15 percent require insulin injections. After delivery, blood sugar levels should return to normal. However, women with gestational diabetes are at increased risk of developing diabetes in the future and of developing gestational diabetes in any later pregnancy.
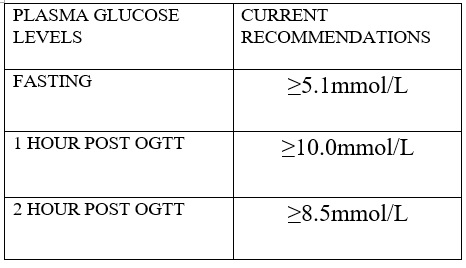
Table 1. Gestational Diabetes Mellitus Diagnostic Criteria
Diet
A pregnant woman with diabetes should follow a diet designed especially for her. Most women with gestational diabetes are referred to dietitians for this. A woman with preexisting diabetes should already be following a special diet; but, she also should get nutritional counseling, as her diet may need modifications as her pregnancy progresses.
As a very general rule, a pregnant woman with diabetes (gestational or preexisting) who is of average weight should consume about 2,200 to 2,500 calories a day. This should help her gain the recommended 25 to 35 pounds during pregnancy.
Home Glucose Monitoring
Pregnant women who are diabetic should monitor their blood sugar levels several times a day. Blood glucose meters or colored strips used with finger-stick devices make it easy to check blood sugar levels.
Leave a reply







