What is Caesarean Section?
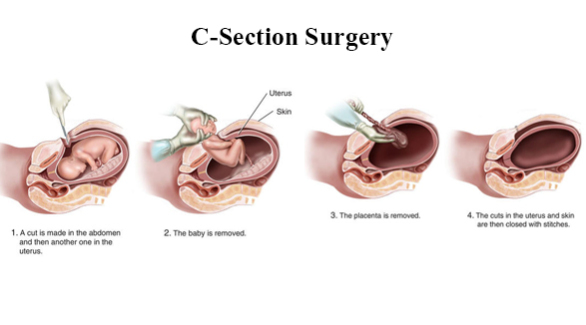
Caesarean section is a surgical operation in which an obstetrician makes an opening in the mother’s abdomen and womb and delivers the baby through it.
When is C-Section indicated?
Caesarean section will only be done in a situation, where a normal vaginal birth may be unsafe for the mother and/or baby. The caesarean section may take place before the mother goes into labour or may become necessary at some point during labour. There are many reasons why caesarean sections may be necessary for some mothers. The common ones include:
- Malpresentation (a situation where the baby is in any position other than head-down). e.g breech presentation (buttock downwards), transverse lie (baby lying sideways)
- Previous caesarean section
- Placenta praevia, whereby a baby’s placenta partially or totally covers the internal opening of the mother’s cervix
- Multiple pregnancy, e.g twins, triplets
- Concern that the health of the mother or the baby is in imminent danger
- Labour is not progressing as planned
- Have heavy or significant vaginal bleeding during pregnancy or labour
- Going into labour before the date of a planned caesarean section
What does it involve?
For an elective caesarean section, you may be given an appointment about one week before the operation during which blood tests may be done to check your red blood cell count and so that blood can be reserved for you if you need a blood transfusion. An anaesthetist may also see you at an appointment prior to your surgery to determine your fitness for anaesthesia and surgery. You will be given either a regional anaesthetic, (which numbs the lower part of the body and means you will be awake during the operation), or a general anaesthetic (where you are made unconscious). This is given by an anesthetist in the operating theatre or in a separate room next to the theatre. You will need to have a catheter inserted to empty your bladder. If you are given a regional anaesthetic, a screen will be placed across your abdomen so that you do not see the operation being done.
During the caesarean section, the operating table will be tilted sideways to an angle of at least 15 degrees so that the uterus is not compressing on the major blood vessels in the abdomen. The obstetrician will make a horizontal cut across your lower abdomen (just below the line of your pubic hair) to reach your womb. This opening along your “bikini line” will cause you less pain afterwards. A vertical cut may be made in a small number of cases (usually if you have had such a cut in a previous operation before). A trained practitioner, skilled in resuscitating newborn babies will be present if your healthcare team has reasons to believe that your baby’s safety is at risk.
What precautions must I take for the procedure?
Please inform your doctor if you have any pre-existing medical illnesses and the medicines that you are taking in pregnancy. Please bring these medicine with you on the day of the operation. Before the procedure, please inform your doctor if any of the following are applicable:
- You have a history of allergy or reaction to any medications, drugs, or food
- You have a history of bleeding or clotting disorders
- You are taking drugs or herbs that thin your blood e.g( Ginko Biloba, Lingzhi, Warfarin, Aspirin, Ticlopidine or Clopidogrel), as these medicines may affect blood clotting and increase the risk of bleeding. If you are taking such drugs, your doctor will advise you accordingly.
- Please let your doctors know about the medicines that you are taking in pregnancy and bring these medicines with you on the day of the operation.
What are the risk and complications of the procedure?
Risks to mother
Common risks:
Infection
You might develop infection which may involve the urine, wound or lung – 6 in 1000 cases. You will be given antibiotics to lower the risks of infections during the procedure. Further antibiotic treatment may be required if subsequent infections develop.
Uncommon risks:
- Excessive bleeding
Eccessive bleeding (usually from the womb) occurs in 5 in every 1000 cases. In the event that you have excessive bleeding, you may require blood transfusion. - Emergency hysterectomy
Emergency hysterectomy (removal of the womb) may be necessary in up to 7 to 8 women in every 1000 based on published studies although our experience suggests a lower rate of less than 2 women in every 1000 cases of caesarean section. This is usually done as a live-saving step in the event of massive bleeding that cannot be stopped by any other means.
Rare risks:
- Injury to the surrounding structures and organs
Bladder injury occurs to 1 in 1000 cases. Ureteric injury occurs to 3 in 1000 cases. These injuries can happen as the structures are very close to the cut that is made in the womb to deliver the baby. Such injuries will be repaired immediately but may require a longer hospital stay. - Deep vein thrombosis (DVT) and/or pulmonary embolism
DVT occurs when a blood clot forms in the vein of the legs or pelvis. This can become life-threatening if the clot dislodges and travels to your lungs. DVT occurs in 4-16 in 10,000 cases. Pregnancy itself is a risk factor for DVT. In addition, the nature of the operation as well as the reduced mobility after a caesarean section (usually due to post-operative pain) can increase the risk of DVT.
Very rare risk:
Death
Death might occur, due to any of the above conditions in approximately 1 in 12,000 cases.
Risks to baby
Common risks:
Cut on the baby’s skin
Sometimes the baby’s skin may be accidentally cut while the opening in the womb is being made. This is usually a small cut that is superficial and will heal without the need for any further treatment. This happened to about 1-2 in 100 babies.
Uncommon risks:
Neonatal respiratory problems
Breathing difficulties just after delivery by caesarean is seen in 35 in 1000 babies, compared with 5 in 1000 babies after vaginal delivery. The baby will need to be admitted to neonatal special care or intensive care for treatment.
Risks to future pregnancies
Uncommon risks:
- Uterine rupture (tear of the womb)
Increased risk of the uterine rupture along the scar of the uterus, during subsequent pregnancies/deliveries happens in 2 to 7 in 1000 cases. This can result in massive bleeding which may be life threatening. - Stillbirth
Increased risk of experiencing a stillbirth in a future pregnancy occurs in 1 to 4 women in every 1000 cases compared to 2 in 1000 cases for women who have has a previous vaginal birth. - Placenta Accreta
A woman who has undergone a caesarean section is at risk of a serious complication called placenta accreta in the next pregnancy if the placenta happens to be in a low position then. In placenta accreta, the placenta does not separate from the uterus as it should when your baby is delivered. If this is the case, you may lose a lot of blood and need a blood transfusion, and you are likely to need a hysterectomy. The risk of placenta accrete increases with each caesarean section ranging from 3 to 1000 cases after one caesarean section (uncommon), to 2 in 100 cases after 3 previous caesarean sections (common).
What are the additional care/treatments for mothers who request for Caesarean Section without a medical indication?
Post delivery, compared to a woman who experiences a vaginal birth, the following are the additional care of treatment for mothers who request for Caesarean Section without a medical indication:
- Longer hospital stay due to increased recovery period
- Increased risk of admission to ICU due to increased risk of requiring further surgery should complications arise
- Pain at the site of the operation
- Additional care of the surgical wound
- Risk of anaesthesia
What can I expect after the procedure?
Immediately after the operation you will be monitored in recovery until your vital signs are stable. If you are recovering well and you have no problems after your caesarean section, you should be able to eat and drink. Your bladder catheter will be removed once you are able to walk and at least 12 hours after the last administration/dosage of your epidural anaesthetic. You will also be encouraged to get out of bed within 12-24 hour of delivery. You may also receive an injection daily to thin your blood to prevent DVT. Unless you have been advised not to, we encourage you to breastfeed and we will assist you. The speed of recovery varies from person to person. In general, women stay in hospital for abut 2 to 3 days. Occasionally women stay longer if there are complications. The time it takes to feel back to normal is approximately 6 weeks. Analgesics and other medications will be prescribed for you to bring home on the day of your discharge. A follow up appointment with your doctor will usually be arranged within 4-6 weeks of your discharge.
Leave a reply








